 As a psychotherapist who has worked as a specialist in gay men’s and HIV mental health for over 23 years, I have always maintained that HIV/AIDS is more than a medical issue; it’s a psychosocial one as well. As Chair of the LA County HIV Mental Health Task Force for 9 years, we advocated for awareness that whatever happened in the course of HIV/AIDS treatment, or in HIV prevention, had implications for mental health and well-being. It’s been a tough fight, sometimes, to get the federal, state, and local governments to recognize this, at every development in the history of HIV in the United States and in Los Angeles in particular. This remains true today, as we cope with the advent of PrEP (pre-exposure prophylaxis, in Gilead’s medication Truvada, the “HIV prevention drug”, which is also used in HIV-positive people as a part of combination therapy).
As a psychotherapist who has worked as a specialist in gay men’s and HIV mental health for over 23 years, I have always maintained that HIV/AIDS is more than a medical issue; it’s a psychosocial one as well. As Chair of the LA County HIV Mental Health Task Force for 9 years, we advocated for awareness that whatever happened in the course of HIV/AIDS treatment, or in HIV prevention, had implications for mental health and well-being. It’s been a tough fight, sometimes, to get the federal, state, and local governments to recognize this, at every development in the history of HIV in the United States and in Los Angeles in particular. This remains true today, as we cope with the advent of PrEP (pre-exposure prophylaxis, in Gilead’s medication Truvada, the “HIV prevention drug”, which is also used in HIV-positive people as a part of combination therapy).
As a somewhat introverted and low-profile local psychotherapist, in private practice now for 17 years (and for many years prior to that as Clinical Director in LA’s local AIDS service organizations), many people still don’t know of me, or what I do. At this point, I am the most experienced openly gay and HIV-positive (25 years!) licensed psychotherapist (LCSW) in LA County who specializes, almost exclusively, in working with gay men and/or those living with HIV.
I am working to change that low profile, because the work I’ve done in the past two decades still needs to be accessed by so many people facing HIV prevention or treatment issues who need help today. Recently, an entire therapy session in my office on San Vicente with a 24-year-old, HIV-negative gay male was devoted to his questions about PrEP. I deferred his strictly medical questions to his physician (with whom I collaborate frequently), but for this client, the psychosocial issues were just as salient. Here is some of what we talked about, which are common topics in gay men’s conversations these days, online and in actual gatherings:
1. Awareness of PrEP – Increasing numbers of gay men are becoming aware of PrEP and moving through the process to gain access and utilize it. While PrEP has been shown in numerous compelling studies (perhaps most famously, the IPREX study) to be reliable and effective, in rates even beyond condoms in efficacy, we have a large portion of the local gay male community who still ask, “What’s PrEP?” Our challenge, as an interdisciplinary, collaborative community of health care professionals, is to increase the level of awareness so that the entire community of gay men (and other especially high-risk populations, such as women of color, transgender people, commercial sex workers, people in serodiscordant (poz/neg) relationships, etc.) can benefit from the outcomes in preventing HIV transmission that PrEP has been shown to give. Health care professionals do this by talking about PrEP to clients/patients, by them talking to each other about it, and so on.
2. HIV Prevention Education — A number of providers who are experienced in HIV lament that the current generation, especially young gay males 14-26, are testing positive in relatively high numbers because they are being exposed to almost no meaningful HIV prevention education, especially publicly-funded, because of the government’s “abstinence-only” and “don’t say gay” public health policies on a federal, state, and local level. Today’s young gay men don’t generally know what AIDS was, how it differs as a term from HIV, and the specifics of HIV prevention strategies. It’s not their fault; they were never really given the opportunity to learn. In the 90’s and even the 80’s, even under (the evil) Reagan, HIV prevention education was MUCH more abundant, sexually explicit, and effective. Los Angeles County alone had public education programs in the early 90’s that were County-funded, informative, fun, and well-attended, and were at least moderately effective in curbing HIV transmission rates compared to what they might have been at the height of the epidemic. Because funding for those “explicit” and gay-specific (aka, culturally competent) educational resources basically dried up by order of the Bush administration and the demands of its socially conservative/religious/anti-gay supporters circa 2001, the provider community must educate the gay community on a one-on-one basis, frequently and specifically assessing patient risk. Young gay men can’t act on what they don’t know, so their receiving frank information about how HIV is – and is not – transmitted becomes imperative. This education, psychosocially, addresses the levels of collective community anxiety about HIV, whether it’s too little (dismissing risk cavalierly) or too much (carrying a phobia about HIV and excessive avoidance of socialization, sex, or relationships in proximity to someone with HIV). In this age of PrEP, additional education needs to focus on differentiating HIV transmission risk and treatment implications, versus “merely” common STD transmission risk and treatment implications. HIV is chronic and requires a lifelong process of continuous treatment, while many STD’s (chlamydia, gonorrhea) are acute and treated (resolved) nearly immediately (while Human Papilloma Virus (HPV), Hepatits C Virus (HCV), and Herpes Simplex Virus (HSV) are more nuanced).
3. HIV Risk Assessment and Management – In the physician/therapist collaboration, the physician is assessing the client’s level of risk via behavioral history and educating the client (time-permitting in your average MD office visit!) on the patient’s risk relative to reported sexual behaviors (and considering the disinhibiting role of drugs and alcohol, too). The psychotherapist is providing psychoeducation about risk, but also exploring the patient’s motivations for behavior. It is well-known that patients with lower self-esteem and/or those who are survivors of molestation or other sexual trauma tend to engage in higher-risk behaviors, which earlier meant non-use or sporadic use of condoms, and in the age of PrEP might mean poor adherence to taking PrEP daily, or not following up with monitoring tests and office visits. Other patients might have not a careless or passive risk, but have a “daring” or active “risk flirtation”. Still others might be having sex that is high-risk for HIV transmission because fluid exchange is just plain “hot” (and intimate) in sex (just ask straight women on birth control pills as their sole contraception method). While the physician can counsel on the medical aspects of risk reduction intervention, the therapist would explore the psychosocial underpinnings and can apply CBT, Behavioral Therapy, Motivational Interviewing, or Harm Reduction (all evidence-based treatments). A therapist would also explore how co-occurring psychiatric disorders might influence sexual risk (Impulse Control Disorder, the hypersexuality of Bipolar Disorder, the lack of self-care in Major Depressive Disorder, maladaptive coping for anxiety, repetition compulsion of sexual trauma/PTSD, substance abuse/dependence, etc.)
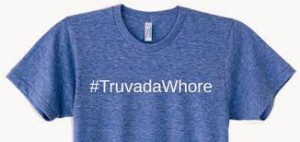
4. PrEP Fear/Resistance/Misinformation/Social Stigma – Even a quick look on social media like Facebook and visitor comments on its popular “PrEP Facts: Rethinking HIV Prevention and Sex” page, with over 5,000 members (founded by pioneering New York psychotherapist Damon L. Jacobs, an admired colleague) will occasionally reveal the presence of at least some “slut shaming” comments about the use of PrEP prophylactically, including from one gay man to another, in an intra-community prejudice that can cause heated discourse. One PrEP advocacy activist made t-shirts that said “Truvada Whore” on them, as a way of taking back the term ironically (much in the way the word “queer” was reclaimed as a term of empowerment for the LGBTQ community years ago). Other comments will reveal heart-felt feelings from gay men who feel “liberated”, psychologically and sexually, after starting PrEP. For some, this is a euphemism that they are no longer using condoms in sex, but are adhering to the recommended use of Truvada as prescribed, and are being monitored in office visits with physicians, which is a perfectly reasonable, scientific HIV-prevention and self-care strategy, despite its popular debate. I myself used alliteration to coin the term that PrEP is “the Chemical Condom,” creating a barrier to HIV not on the penis, but in the bloodstream. For others, they are using PrEP in addition to condoms. They are sometimes confronted with, “But isn’t that overkill? Isn’t that like a woman using the pill, a diaphragm, and an IUD to prevent pregnancy?” The emphasis on personal choice and empowerment doing what feels comfortable on an individual basis is a running theme.
Many gay men reveal a feeling of hope that perhaps gay men’s sex can finally return to a time of “pleasure” that was enjoyed throughout history and until the late 1970’s/early 80’s, when condoms were not used but STD’s were monitored and treated quickly (many people don’t know that the current LA LGBT Center, the largest gay non-profit organization, was founded after “Stonewall” and its early “community services” focused on STD testing and treatment). What is significant is that these social media comments both for and against PrEP are expressed fervently, whatever the opinion is. This means that in doctor-patient discussions, patients will likely have strong, “deeply-held beliefs” (a popular but controversial term these days) and the responses from all health care and social service professionals need to validate at the least the passion behind their expressions, even if we might educate or challenge the content of them.
Another factor, which speaks to #2 above, is that much specific mis-information exists; some patients strongly argue on points that the latest research on PrEP (and even much older research) refutes. Our ability to inform, dispassionately, about what research is (let’s start with that; many patients are unfamiliar with all forms of peer-reviewed, empirical research, and how it is valid/reliable) and what that research has said, is imperative. Education, validation, the opportunity for patients to feel heard and ask questions, and the opportunity for them to be re-educated, or to have their dearly-held “facts” at least qualified, is important in communications between patient/client and health care providers. This means that health care providers (physicians, social workers, other types of therapists, nurses, treatment advocates, health educators, etc.) really need to know their stuff on a current, razor-sharp, cutting-edge basis. Much of the new data might confuse patients on what they previously learned, such as the largely debunked concepts of “re-infection” or “super-bug” that were part of discourse not that long ago. Concepts like TasP for HIV-positive patients (Treatment as Prevention, aka “undetectable = non-transmissible”) directly contradict previous public health messages. Having to learn and re-learn facts about HIV is challenging in our information-overload era. This is compounded for people for whom English is a second language, or for whom all this “biology” discussion is beyond their formal education, aptitude, or interest.
5. Access/Affordability of PrEP – For other patients, issues of how to access PrEP in the context of the status of whether they have health insurance, or a health insurance plan with prescription drug coverage, will be of concern, as well as their ultimate out-of-pocket expense when picking up their prescription. Resources like the Gilead co-pay patient assistance program should be discussed. For physicians who simply “don’t have time” to discuss administrative issues on patient benefits, referral to a therapist knowledgeable in gay and/or HIV local resources (such as myself, or anyone with good old-fashioned social work case management skills) can help with this, from initial awareness/access to long-term follow-through and adherence. While a physician’s (or other provider’s) focus might not be on the affordability of care, such as the cost of insurance premiums, office visit co-pays, co-insurances, prescription co-pays, or even medical building parking fees, we can be sure patients are thinking about them. It all goes into the mix of making things practical and workable, and as a health care system, we have a LONG way to go on these. I believe MOST people find medical (and related) services a strain to afford on an ongoing basis. Fortunately, many patients on PrEP find ways that it’s affordable, and it is in the public’s interest that it be made affordable and accessible. After all, from a public health funding perspective on HIV, “an ounce of prevention is worth a (ton) of cure”.
6. Adherence to PrEP – Just as adherence to HAART (highly-active antiretroviral therapy, or “combination drug” therapy) was (and is) a big issue for successful and continuous viral suppression in HIV treatment (and avoiding HIV breakthrough and viral resistance), adherence to PrEP is important. While there is some data that implies “partial efficacy” in partial adherence, daily use brought the efficacy of PrEP in trials up to nearly 100 percent. I have given presentations and written articles on the cognitive-behavioral tools that can enhance HAART adherence for HIV-positive patients, and they apply to HIV-negative patients on PrEP as well. Adherence is both a behavioral (practical) issue and a psychological one. Patients with co-occurring adult ADHD, for example, might have more challenges paying attention to a daily pill schedule, while patients with OCD might astound providers with exceptional adherence (not missing a dose in a year, for example). Co-occurring substance abuse (particularly methamphetamine) and/or Major Depressive Disorder can negatively affect adherence. If someone has adherence issues for any aspect of HIV treatment (and really for any other disorders, too), a course of Behavioral Therapy from a qualified and culturally-competent therapist can help improve this.
7. Implications for the Future – For over 9 years as the Chair of the LA County HIV Mental Health Task Force, I co-chaired (with others, especially Tom Donahoe, MBA, of the UCLA/Pacific AIDS Education and Training Center) the annual “Coping with Hope” HIV Mental Health Conference in Culver City. Coined in Task Force meeting discussions, the term originated with how we, as a community of HIV service providers and consumers, “coped” with the new-found hope for extended life that the advent of HAART brought to the world. While most of it was wonderful, the advent of HAART was not without its psychosocial challenges, particularly around concerns about access, adherence, and long-term effectiveness. So it is the same with PrEP. Can the current (and future) generations of gay men go back to condomless sex (as if it every really went away) without fear of HIV? Can we put (finally) the entire “episode” of the decades-long “AIDS Crisis” behind us, and approach sex more confidently and less anxiously than we have in decades? Others fear a phantom public health catastrophe from a return to condomless sex, as if it were the mere “promiscuity” and sexual “abandon” of the 70’s “gay liberation movement” alone that “tempted God” and brought about the wrath of the AIDS crisis as divine punishment, and not the presence of HIV itself as a biological phenomenon. It is extremely difficult to separate fear, rumor, posturing, judgment, envy, stigma, religiosity, and moralism from the purely medical and scientific on any public health issue (women and birth control, “morning-after” pill, HPV vaccine, comprehensive sex education, etc.). But it is only through a collaborative, comprehensive, integrated, and multi-disciplinary approach among providers (including between physicians and psychotherapists) that we create an optimal public health response to HIV, integrating the medical and the psychosocial. The advent of PrEP in the mix is no different.
Are we meeting the current challenges? Maybe not fully. But we’re coping with the hope that one day, we can.
If I can be of supportive consultation to you, or to your organization, corporation, media project, or school, I’m available at 310-339-5778, or Ken@GayTherapyLA.com.
*********************************************************************************************************************
Ken Howard, LCSW, is a gay and HIV-positive (29 years) licensed psychotherapist (LCSW) and life/career coach who has specialized in working with gay men, as individuals and couples, for over 27 years. He helps many gay men (and others) resolve the issues that undermine your quality of life, and helps you to thrive.
For help improving your personal or professional life, whatever your current challenges are, consider sessions with Ken for counseling, coaching, or therapy sessions, at his office in Los Angeles/West Holllywood (near Beverly Center mall), or via phone, or via webcam, anywhere in the world. Call 310-339-5778 or email Ken@GayTherapyLA.com for more information.
Ken is also available for expert witness work on legal proceedings involving gay issues, all LGBT issues, HIV issues, and issues concerning psychiatric illness or disability, as well as organizational consulting for non-profit organizations, corporations, college campuses, and conferences.
To get your copy of his self-help book, Self-Empowerment: Have the Life You Want!,visit www.Amazon.com , or wwwLuLu.com. It’s your “portable therapist” for the challenges you face today in your mental health, health, career, finances, family, spirituality, and community.
